It didn’t happen overnight. It wasn’t a fluke. The fastest vaccine development in history was decades in the making—and it may just change the future of medicine.
Before the Breakthrough
For most of human history, infectious diseases were nature’s cruelest weapon. Polio, smallpox, influenza, HIV—these weren’t just illnesses, they were eras. Wars paused for them. Economies collapsed under them. Lives were measured by how soon someone you loved would be taken.
Vaccines changed that. But traditional vaccine development is slow. It takes years—sometimes decades—to grow viruses in eggs or cell cultures, inactivate them, purify them, and test them. That’s how things were done… until a radically different idea came along.
What if we didn’t need to give people bits of a virus at all?
What if we could just teach the body to build its own defense?
The “Impossible” Idea
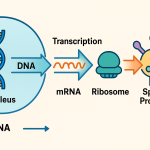
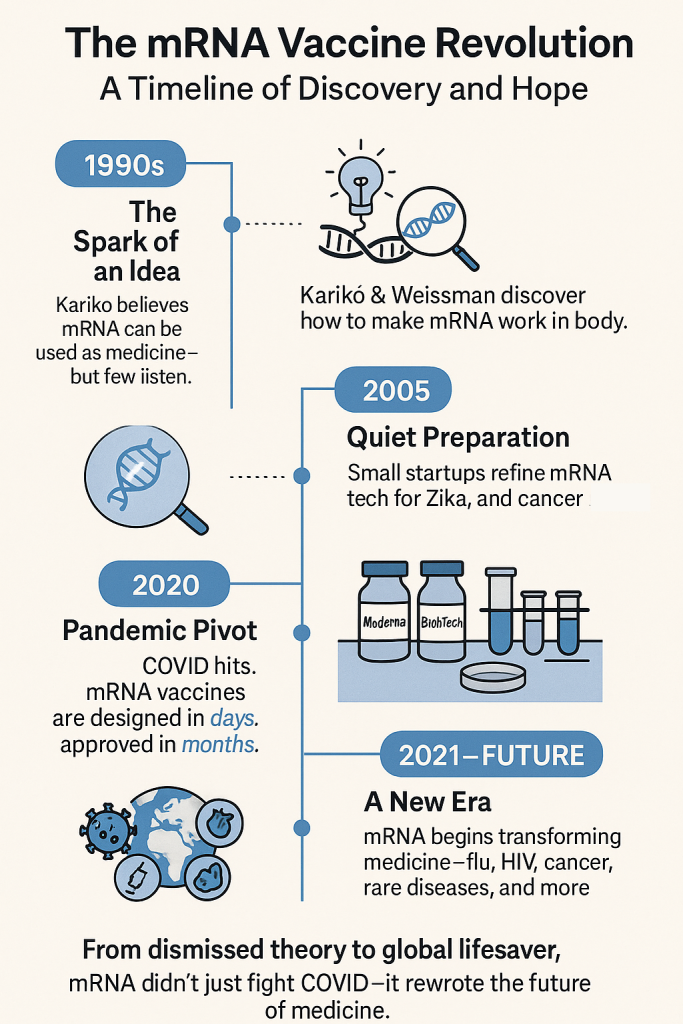
In the 1990s, Hungarian-born biochemist Katalin Karikó was obsessed with a molecule called messenger RNA (mRNA)—the simple genetic courier that tells your cells what proteins to make. She believed mRNA could be used like software: feed it into the body, and it would program your own cells to produce the exact protein needed to trigger an immune response.
But most scientists thought it was a dead end. When you inject synthetic mRNA into the body, the immune system usually destroys it before it can do anything. Research grants dried up. Karikó was demoted. She was told—more than once—to give up.
But she didn’t.
She teamed up with immunologist Drew Weissman at the University of Pennsylvania. Together, they discovered a crucial tweak: by modifying one of the RNA bases—pseudouridine instead of uridine—they could sneak the mRNA past the body’s defenses and get it to do its job. That 2005 discovery laid the foundation for the entire field of mRNA therapeutics.
At the time, no one noticed. Scientific journals rejected the paper. Pharmaceutical companies weren’t interested.
But a few people were paying attention.
The Silent Race
Two small biotech startups, Moderna (founded in 2010) and BioNTech (founded in 2008), quietly began developing ways to turn mRNA into medicine. Their scientists experimented with mRNA-based vaccines for flu, Zika, and cancer. They were refining the manufacturing process, testing delivery systems (like lipid nanoparticles), and building a platform that could pivot quickly to new threats.
Still, by early 2020, no mRNA vaccine had ever been approved for use in humans.
Then came a virus.
The Perfect Match
When SARS-CoV-2 emerged in late 2019, scientists around the world scrambled for answers. But this time, we had a new tool. The genetic sequence of the virus was published online on January 11, 2020.
Within 48 hours, Moderna had designed an mRNA vaccine.
Within a few weeks, BioNTech partnered with Pfizer to do the same.
Because mRNA vaccines don’t require growing viruses in labs, production could scale rapidly. No waiting on egg-based cultures or months-long manufacturing delays. Clinical trials began in record time. And by December 2020—less than a year after the virus was sequenced—the first mRNA vaccines were saving lives.
That had never happened before in the history of medicine.
What mRNA Vaccines Gave Us
They didn’t just work. They worked exceptionally well. In clinical trials, the Pfizer-BioNTech and Moderna vaccines showed more than 90% efficacy at preventing symptomatic COVID-19—an almost unheard-of result in vaccine development.
And they were incredibly safe.
Billions of doses later, real-world data confirm what the trials showed: these vaccines prevented millions of hospitalizations and deaths. They helped societies reopen. They gave families back their holidays. They gave grandparents back their grandchildren.
But that’s just the beginning.
What’s Next for mRNA?
Today, mRNA is being tested for everything from influenza to RSV, malaria, and even cancer. Because it’s a platform—not a one-off solution—it allows scientists to design, test, and manufacture new vaccines faster than ever.
Here’s what’s in development right now:
- A universal flu vaccine that could protect against all strains in one shot
- Personalized cancer vaccines, built from a patient’s own tumor profile
- A vaccine for cytomegalovirus (CMV), a common but dangerous virus during pregnancy
- Experimental vaccines for HIV, dengue, tuberculosis, and more
And because mRNA is so flexible, it could eventually help treat autoimmune diseases, rare genetic disorders, and even heart disease, by programming cells to produce healing proteins.
It’s not just vaccines—it’s programmable medicine.
The Future We Almost Didn’t Get
None of this would have been possible without decades of research, mountains of failures, and people who refused to quit.
Katalin Karikó and Drew Weissman finally received the Nobel Prize in Medicine in 2023. By then, their work had already saved millions of lives.
mRNA vaccines are a triumph—not just of science, but of persistence. Of quiet, underfunded brilliance. Of staying curious. Staying stubborn. And believing, even when the world doesn’t.
From Pandemic to Possibility
When the COVID-19 pandemic hit, it didn’t just take lives. It tested our trust—in science, in institutions, in each other. But out of that test came one of the greatest public health breakthroughs in history.
mRNA technology turned the tide. And it’s still just getting started.
The future of medicine might not come in a pill or a bottle.
It might come in code.
Wrapped in a nanoparticle.
Ready to teach your body how to fight.
That’s how the world got better.
And how it may get better still.
Our ‘When The World Got Better’ Series
- When The World Got Better: Smallpox
- When The World Got Better: Polio
- When The World Got Better: Measles
- When The World Got Better: HBV
- When The World Got Better: Hib vaccine
- When The World Got Better: mRNA vaccines
- When The World Got Better: Influenza
Last Updated on June 30, 2025