Part 3 of 3: Why Herd Immunity Is About More Than Just You
About this Series
This article is part of a series designed to help readers think clearly and calmly about vaccines. In an age of misinformation and overwhelming noise, we aim to cut through the confusion with evidence, reason, and empathy. Whether you’re vaccine-hesitant, curious, or just want to make informed choices for your family, this series is here to offer clarity—grounded in science, not fear.
- Part I – You’re Asking the Wrong Question
- Part II – Not All Risks are Equal
- Part III – You’re Not Alone in This Fight
Imagine you’re walking through a forest at the end of a long, dry summer.
The air is still. The trees are tall. The underbrush is thick with dead leaves and fallen branches—fuel just waiting for a spark.
You strike a match.
If that match lands in a bed of dry kindling, it might ignite something catastrophic—a wildfire that spreads from tree to tree, consuming everything in its path.
But if that match lands in a clearing where the ground has been swept clean, it fizzles. No blaze. No destruction. Just a puff of smoke and a near miss.
Now imagine that same match is a virus. And the kindling?
That’s us—the people in a community who are susceptible to infection.
💉 Vaccines Don’t Stop the Spark. But They Remove the Fuel.
When most people think about vaccines, they think about individual protection:
- Will this shot keep me from getting sick?
- What are the side effects?
- Do I personally need it?
These are reasonable questions. But they miss something big: vaccines don’t just protect you—they protect the people around you. They change how a virus spreads through a community.
This idea is called herd immunity, and it’s one of the most powerful tools public health has ever developed. But it only works if enough people participate.
🔄 The Chain Reaction You Don’t See
Viruses spread by hopping from person to person—through breath, touch, sneezes, surfaces. Every infected person is a lit match, and every unvaccinated, susceptible person is a dry patch of kindling.
If the fire hits someone who’s vaccinated, it usually stops cold. That person’s immune system smothers it before it can move on.
But if it hits someone who isn’t protected, it catches—and the fire continues.
And here’s the most important part: you don’t need to feel sick to be spreading the flame.
Some of the most dangerous outbreaks in history were fueled by people who felt fine but were carrying the virus anyway.
That’s how community spread works: it’s invisible until it’s everywhere.
🧩 Herd Immunity: How It Actually Works
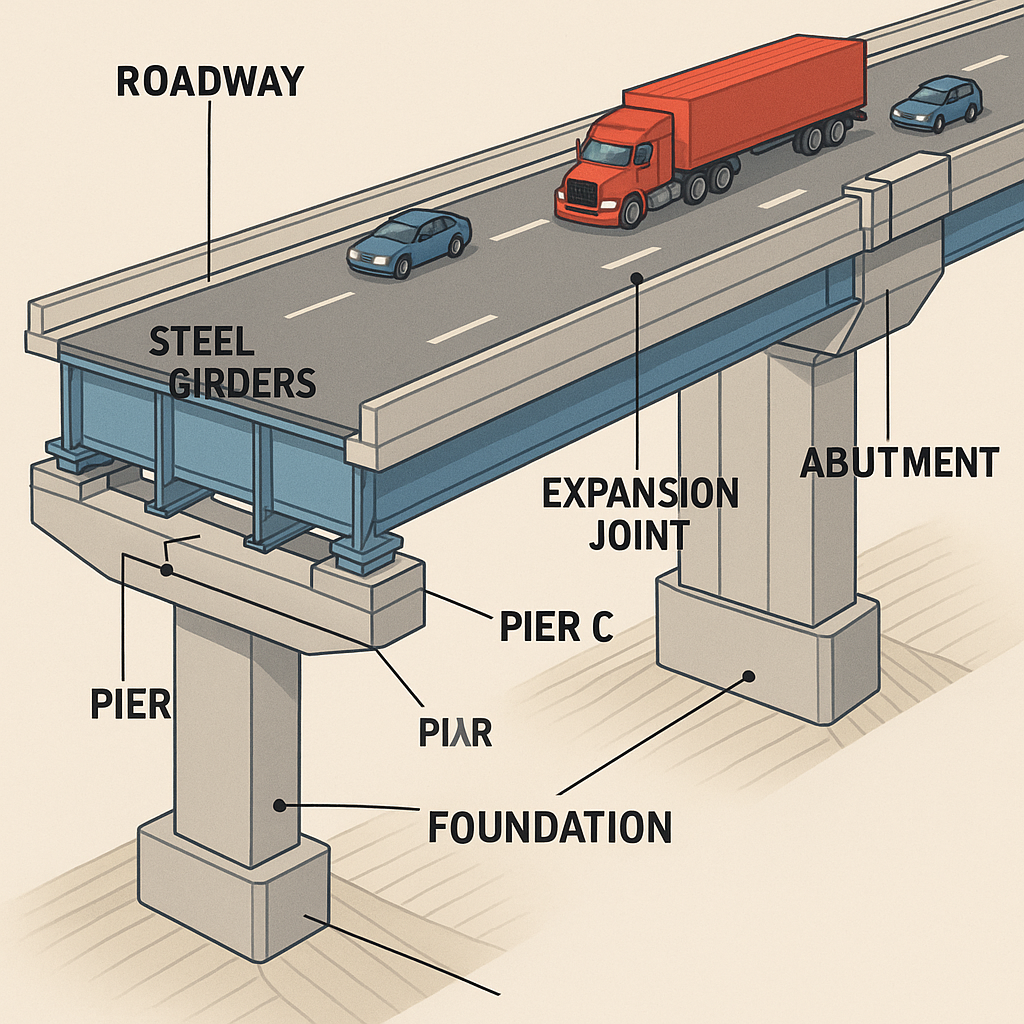
Herd immunity isn’t just a nice idea—it’s math.
Every virus has a number called R₀ (R-naught)—the average number of people that one infected person will go on to infect in a totally unprotected population.
- For measles, R₀ is sky-high: around 12 to 18
- For the original COVID-19 strain, it was around 2 to 3
- For newer variants like Omicron, it jumped to 8 or more
The higher the R₀, the more people need to be immune to break the chain.
For measles, you need over 95% of the population vaccinated to prevent an outbreak. For COVID, the threshold varies with the variant, but the principle is the same: the more people who are immune, the harder it is for the virus to find a host.
Every vaccinated person is like clearing a patch of fuel from the forest floor. Enough of those, and the fire has nowhere to go.
🧠 Wait—Don’t Vaccines Need to Stop Transmission for Herd Immunity to Work?
Not entirely. No vaccine completely halts transmission—not even the ones for measles or polio. What vaccines do is reduce the chance that you’ll get infected, and if you do, you’re often less contagious for a shorter time. That still slows the spread.
And slowing the spread matters. Even if transmission isn’t eliminated, fewer infections means fewer hospitalizations, fewer deaths, and less chance for the virus to reach those most at risk.
Herd immunity doesn’t require 100% immunity. The goal is to bring the virus’s effective reproduction number (Rₑ)—how many people each infected person passes it to on average—below 1. Once that happens, outbreaks naturally burn out. We can get there with a mix of partial immunity, safer behavior, better ventilation, and yes, vaccines.
So even imperfect protection can still shift the tide.
🧓 Who You’re Protecting
Let’s make this personal.
Some people can’t be vaccinated—like newborn babies who are too young, or individuals with severe allergies to vaccine components.
But many others can get the shot and still remain vulnerable—because their immune systems aren’t strong enough to respond fully.
- A woman undergoing chemotherapy, fighting to survive long enough to see her kids graduate from college.
- A transplant recipient whose immune system is deliberately suppressed to protect a life-saving organ.
- A man with advanced HIV.
- A child with a rare autoimmune disease.
They may do everything right—masking, distancing, getting every dose they can—and still be left exposed.
💭 Now, imagine it’s you.
You’re sitting in a hospital chair, an IV pumping chemotherapy into your veins.
The cancer diagnosis was the worst news of your life—but you’re determined to beat it.
You dream of holding your future grandchildren. You want more time. You’re doing everything you can to stay alive.
But as you look out the window, you realize: your odds don’t just depend on your doctors. They depend on strangers—people you’ll never meet—choosing to care about you.
You can’t make their choice for them.
All you can do is hope that someone out there—someone healthy and free—chose to get vaccinated.
Not only for themselves.
But for you.
🌍 The Young and Healthy Still Matter
You might think:
“I’m young and healthy. If I get sick, it won’t be that bad.”
And that might be true. But it doesn’t mean you’re not part of the equation.
In fact, people with strong immune systems and active social lives are often the biggest spreaders—not because they’re careless, but because they’re mobile. They travel. They go to school, the gym, the office, the coffee shop. They interact with dozens or hundreds of people in a typical week.
If you catch the virus and fight it off with barely a sniffle, you might not even know you had it. But in the meantime, you could pass it to your coworker… who passes it to their elderly parent… who ends up in the hospital.
That chain began with you—even if you never saw the spark.
🔬 Real-World Proof: What Happens When Herd Immunity Breaks
We’ve seen what happens when vaccination rates fall.
- In 2019, a measles outbreak in Washington State sickened dozens of children in a community with low vaccine coverage.
- During the early days of COVID-19, we watched entire healthcare systems buckle under the strain of uncontrolled spread—largely because the virus reached vulnerable people through healthy ones.
Viruses are opportunistic. They don’t need everyone to be unvaccinated—just enough.
When enough kindling is left lying around, the spark becomes a blaze.
❤️ Vaccination Is an Act of Compassion
We talk a lot about freedom when it comes to healthcare choices. But there’s another kind of freedom that matters, too:
- The freedom of a parent to send their newborn to daycare without fear of polio.
- The freedom of a cancer patient to go to the grocery store without dodging COVID.
- The freedom of a teacher with lupus to stand in front of a classroom without worrying about who’s carrying measles.
When we vaccinate, we’re not just protecting ourselves. We’re clearing the underbrush. We’re creating firebreaks. We’re holding the line for the people who can’t.
And that’s not weakness. That’s strength.
🔚 Final Thought: You’re Part of the Firebreak
You might never know the spark that starts the next outbreak.
You might never meet the person your immunity protected.
And you’ll never see the harm you helped prevent—because it didn’t happen.
That’s the paradox of prevention: when it works, it’s invisible.
There’s no headline that says “Virus Doesn’t Spread Thanks to You.”
No alert when your body stops a pathogen from reaching your neighbor.
No news story when an outbreak fizzles because there just weren’t enough susceptible people left to sustain it.
But that absence—that non-event—is the point.
It means the baby wasn’t hospitalized.
It means the teacher stayed healthy.
It means the chemo patient finished treatment and lived to meet her grandchildren.
And you were part of that.
In a world where infectious diseases still roam, choosing to vaccinate isn’t just a personal health decision—it’s a quiet act of protection. A firewall. A gesture of compassion for people you’ll never meet.
You don’t have to be a doctor. You don’t have to be a scientist.
You just have to be a break in the chain.
So the next time someone asks, “Why should I get vaccinated if I’m not at risk?”—
Tell them:
“Because maybe someone else is. And maybe I’m their firebreak.”
📚 References
- Centers for Disease Control and Prevention (CDC)
- World Health Organization (WHO)
- Johns Hopkins Bloomberg School of Public Health
- National Cancer Institute
- Nature Medicine (Peer-Reviewed Journal)
- Risk of Long COVID After Breakthrough Infection (2022)
https://www.nature.com/articles/s41591-022-01840-0
- Risk of Long COVID After Breakthrough Infection (2022)
Last Updated on July 7, 2025